In a major leap forward for cancer treatment worldwide, scientists in China have developed a highly scalable and cost-effective way to mass-produce powerful immune cells capable of targeting and destroying cancer cells — a development that could help overcome one of the biggest bottlenecks in cancer immunotherapy.
Researchers at the Chinese Academy of Sciences unveiled a revolutionary method that transforms a single early-stage stem cell into millions of natural killer (NK) cells — specialized immune cells known for their ability to identify and kill abnormal cells such as cancer. By starting with CD34+ hematopoietic stem and progenitor cells from donated umbilical cord blood and genetically engineering them before they fully mature, the team achieved unprecedented expansion of NK cells and CAR-engineered NK cells in the laboratory — up to 14 million tumor-killing cells from just one stem cell.
The significance of this breakthrough stems from how traditional NK cell immunotherapies are manufactured. Conventional approaches rely on mature NK cells extracted from donors’ blood or cord blood, which vary widely in quality, are difficult to genetically modify, and require intensive processing and high costs. This has limited the availability, scalability, and affordability of cellular immunotherapies, especially in resource-limited settings.
In contrast, the new method engineers immune cells at the earliest stage of cell development, allowing the genetic modification — including the addition of chimeric antigen receptors (CARs) that direct the cells to target specific tumor types — to be passed on to millions of descendant cells as they proliferate. This dramatically increases the yield of potent cancer-fighting cells while significantly reducing the amount of viral vector material required for genetic modification, which is one of the most expensive aspects of current CAR-cell therapies.
In preclinical tests, both the induced NK (iNK) cells and CAR-equipped iNK cells generated by this process demonstrated strong anti-tumor activity in laboratory models of leukemia, slowing tumor growth and extending survival in mice. Researchers say that the large quantities of cells produced could eventually enable “off-the-shelf” immunotherapy products — meaning clinics might have ready-to-use cell therapy doses without needing to custom-manufacture cells for each individual patient.
Experts in immunotherapy say this development could significantly lower barriers to access for advanced cancer treatments that harness the body’s immune system, such as CAR-NK and CAR-T cell therapy. Currently, these therapies can cost hundreds of thousands of dollars per patient and are limited to a small number of specialized medical centers. By enabling production at scale, the new technique may help democratize access and expand usage globally.
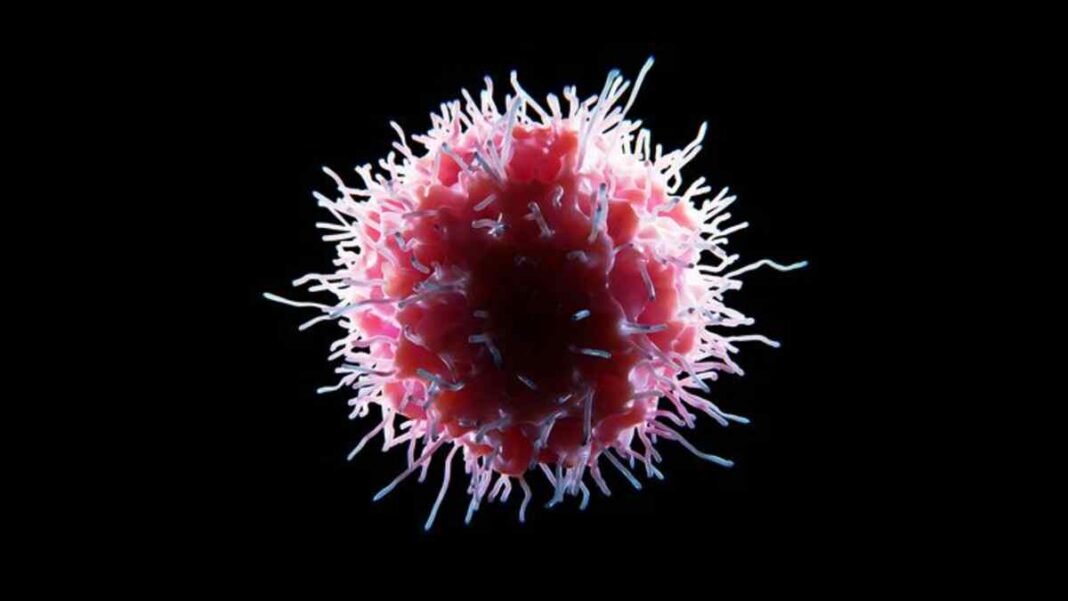
Natural killer cells are a critical component of the innate immune system; they act as first responders that detect and eliminate cells exhibiting abnormal changes — such as cancerous mutations — without prior sensitization. When engineered with CARs, NK cells gain the ability to recognize specific tumor markers, leading to more precise and effective targeting of cancer cells.
While clinical trials in humans are still needed to confirm safety and efficacy, the scalable production platform could help bring such trials closer and speed up the development of next-generation cell-based cancer therapies. Researchers say the approach could also support repeat doses of treatment — a key advantage in treating aggressive cancers where sustained immune pressure may be necessary to achieve remission.
Global cancer researchers are watching closely, as this breakthrough addresses one of the field’s longstanding challenges: how to produce sufficient quantities of engineered immune cells for widespread therapeutic use. If successful in clinical settings, the technique could reshape how cancer immunotherapy is delivered, making high-impact treatments more affordable and scalable for patients around the world.